What are osteopenia and osteoporosis?
These are conditions that cause bones to become weaker and more brittle. Osteopenia can be a precursor to osteoporosis and with treatment can be prevented from getting worse. Not everyone with a diagnosis of osteopenia will go on to develop osteoporosis.
Many older people develop osteoporosis. Women are at a greater risk, which increases further after the menopause – particularly in women who started their menopause before the age of 45.
Risk factors for osteoporosis include:
- being overweight
- low body mass index
- family history of osteoporosis
- smoking
- heavy alcohol intake
- lack of weight-bearing exercise
- long-term use of steroids (corticosteroids)
- low levels of calcium or vitamin D.
Does HIV cause bone problems?
People living with HIV have more incidences of bone mineral density loss and fragility fractures. Opinion is divided on whether this is because of the virus itself, side effects of treatment or inflammation.
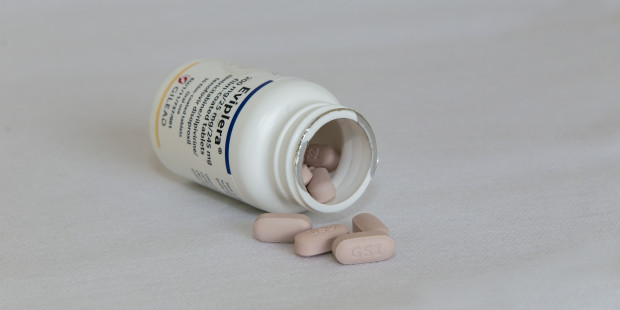
However, bone mineral density has been found to decline by 2-6% in the first couple of years after starting antiretroviral treatment. In particular, the old formulation of tenofovir, as well as the protease inhibitor class, tend to show links with bone density loss, which usually improves when the regimen is switched.
One study found that people with low bone density who were taking tenofovir disoproxil fumarate (TDF) – which is the old formulation – showed an improvement in bone health when switching to the new formulation, tenofovir alafenamide (TAF).
Other traditional risk factors for osteoporosis – like smoking, low body weight, drinking alcohol and low levels of testosterone – tend to be more common in people living with HIV.
Monitoring bone health
If you’re aged over 50, you should be screened for a risk of bone fractures (this should be done earlier, when you are over 40, if you have a major risk factor).
DEXA scanning (a type of X-ray which can identify bone density loss) should be offered by your HIV clinic if you’re a post-menopausal woman, aged over 50 (regardless of sex), or if you’re at a high risk of fractures, whatever your age.
How is osteoporosis treated?
Treatment involves trying to strengthen your bones and prevent fractures through:
- medicine
- lifestyle factors such as weight-bearing exercise.
There are a range of treatment options available including bisphosphonates, strontium ranelate and selective oestrogen receptor modulators (SERMS). Your clinician will look at the best treatment for you and may also suggest calcium and vitamin D supplements or, in the case of menopausal women, hormone replacement therapy.
Lifestyle changes
According to NHS Choices, increasing the amount of weight-bearing exercise you take can increase your bone density. This includes activities such as walking, dancing, running or low-impact aerobics. Exercises such as swimming and cycling are not weight-bearing, but are great for overall health.
It’s best to get advice from a doctor or physiotherapist at your clinic before starting an exercise programme. This is because the type of exercise recommended may vary depending on your level of bone density loss and whether you have had any fractures or not.
Eating a healthy and balanced diet will help you get all the vitamins and minerals you need and help to strengthen your bones. It’s important to eat enough food containing calcium, which strengthens bones, and vitamin D, which helps your body to absorb calcium. Sunshine can also increase your levels of vitamin D.
The National Osteoporosis Society suggests that getting around 10 minutes of sunshine (a bit longer if you are Black or Asian) once or twice a day on bare skin (without sunblock, but taking care not to burn) will help your body make vitamin D.
It may be a good idea to book an appointment with a dietician and physiotherapist at your HIV clinic to get further advice.