The Positive Perspectives 2 study (2020) surveyed 2,389 people living with HIV from 25 countries including 123 from the UK. It found that 801 (34%) had not been told about Can't Pass It On/Undetectable = Untransmittable (U=U) by their healthcare professionals, and men who have sex with women were the group least likely to report having been given this information.
The 1,588 (66%) who had been informed by healthcare professionals were more likely to believe that effective treatment prevents transmission, to report treatment satisfaction, to have an undetectable viral load and to report better general, mental and sexual health.
The Positive Perspectives Policy Manifesto (2020) that resulted from this study states: 'It is clear from the study that there is urgent concern that healthcare professionals should use a common scientific discourse on U=U that is both evidence-based and free from bias and any other prejudices which may be held by the healthcare professional.
'Despite guidelines from professional organisations, accurate and unambiguous reassurances have not been integrated into routine clinical practice of all healthcare professionals.'
Our research on the impact of U=U for patients
Following on from research conducted by the British HIV Association among its members in 2018 that highlighted the lack of consistency about how the U=U message was shared, we aimed to better understand what impact this was having from a patient’s perspective.
An online survey for people living with HIV was created that was live for four weeks in November/December 2019 and was advertised on social media, posted on UK-CAB’s message board and promoted via our networks. The survey collected qualitative and quantitative data about how people who are living with HIV heard about U=U, what they were told and what they felt about it.
Survey results
- 309 people living with HIV completed the survey.
- 250 of respondents were male (80.9%), including two trans men.
- 50 (16.2%) were female, including two trans women. Five (1.6%) were non-binary and four (1.3%) were ‘other’.
- 218 (70.6%) were gay men, 1 (0.3%) was a lesbian, 57 (18.4%) were heterosexual, 20 (6.5%) were bisexual, eight (2.6%) were ‘other’ and five (1.6%) preferred not to say.
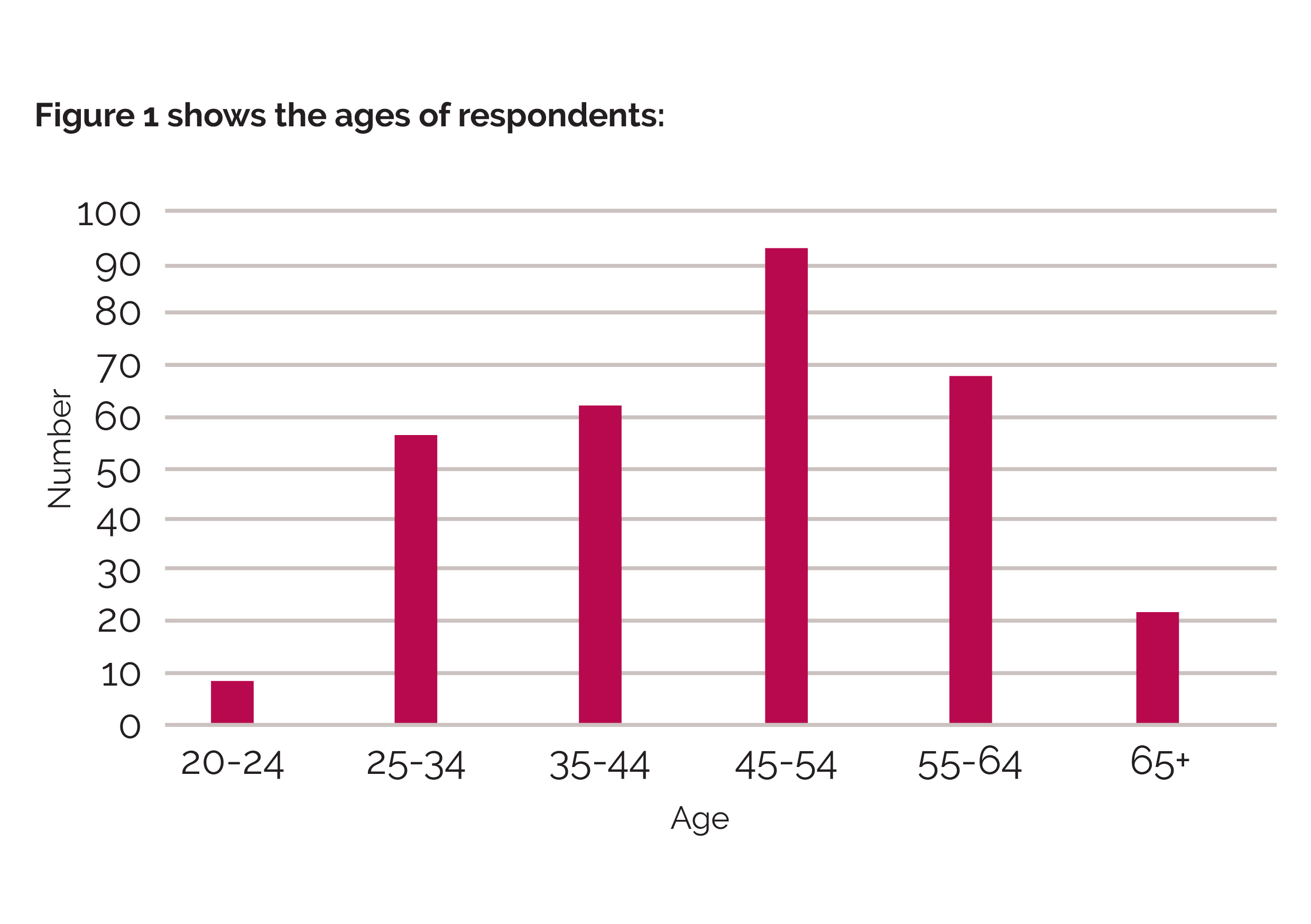
- 202 (66%) were white British, 33 (11%) were black African, 30 (10%) were white and other, and 15 (5%) were white Irish. Fourteen other ethnicities made up the remaining 8% of the sample with 29 people.
- 151 (49%) of respondents were diagnosed over 11 years ago, 60 (19%) were diagnosed 6-10 years ago and 98 (32%) were diagnosed in the last five years. (For the purposes of our analysis, those diagnosed in the last five years were defined as recently diagnosed and those diagnosed 11+ years ago were defined as long term diagnosed.)
- 95% of respondents reported having an undetectable viral load.
- All respondents reported that they knew about U=U.
Only 39% of respondents reported that their healthcare professional said that an undetectable viral load meant a zero risk of transmission.
There were a number of differences between those who were recently diagnosed and the long term diagnosed in terms of the impact of the message and individual people’s experiences:
- 91% of the recently diagnosed said they could have sex without worrying about transmission compared to 80% of the long term diagnosed.
- 74% of the recently diagnosed said it motivated them to take treatment compared to just 49% of the long term diagnosed.
- Only 41% of both recently diagnosed and long term diagnosed said it gave them the confidence to disclose.
Key learnings from the survey
Reassuringly, everyone who answered our survey knew about U=U and respondents clearly demonstrated the importance of the U=U message for people living with HIV.
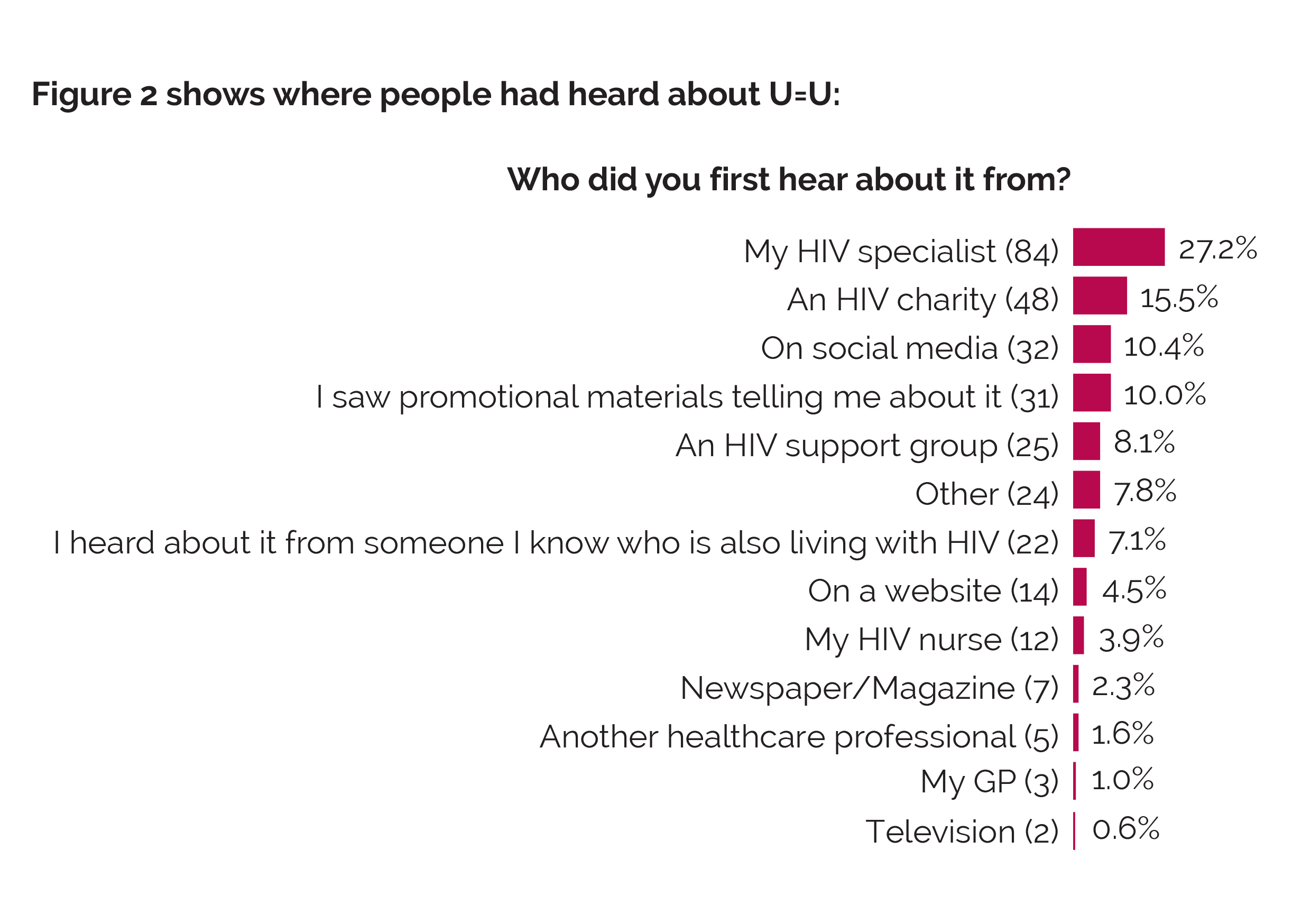
Most people are finding information about U=U from outside of the clinic setting and this demonstrates the importance of ensuring there are multiple sources of information available.
The clinic setting remains an important source of information and our survey demonstrates that there is still a considerable lack of consistency and definitive language around U=U from healthcare professionals.
This highlights the need for all healthcare professionals to follow BHIVA guidelines when talking about U=U and reinforce these messages regularly and consistently when they meet with their patients and not to assume that their patients either fully understand or believe it. This should include GPs and other medical professionals, not just HIV clinicians.
What we learnt from this survey has informed the development of this training.
Quotes from the survey
Recently diagnosed white British heterosexual woman, aged 62:
'I think it should have been explained to me when I was diagnosed, i.e. that with treatment I would become undetectable and what that means. Not knowing probably contributed to my own self stigma and my confidence about sharing my status with others. I think this also probably contributed to feelings of isolation.'
Long-term diagnosed white British heterosexual woman, aged 48, who had only found out about U=U six months before the survey:
'I wish I had known sooner. I’d have liked to have known that I wasn’t a risk to my husband, and haven’t been for 10 years. Reading about it in my clinic waiting room was quite a public way to find that out!'

